State Of Emergency Over Deadly Hepatitis A Outbreak
“California declared a state of emergency Friday (October 13th, 2017) after a deadly Hepatitis A outbreak has spread faster than the state’s ability to supply the vaccine that can ward off the disease.” says Jack Davis over at westernjournalism.com. A “state of emergency” says it all; in the entire year of 2015 there were 1390 cases reported nation-wide (the latest statistics available by the CDC as of this writing). This outbreak has already claimed 17 lives from the 569 people who have been infected and just in the in Southern California area and just over the past 11 months.
What is Hepatitis A and How Did I Get Infected?
Hepatitis A communicable disease of the liver caused by a virus (Virus vs Bacteria Article Coming Soon). That “communicable” word is a pretty fancy way of saying that it’s, “able to be communicated to others” or can spread from person to person. It’s not really something that you “get” from your dog, cat or mosquitoes. No, you’re not going to get Hepatitis A by just talking to someone with Hepatitis A either. Hepatitis A is spread through the fecal-oral route. Yep, you get Hepatitis A by getting someone else’s poo-poo in your mouth. How gross is that?!
If you are asking how in the world does someone get poop in their mouth, this possible scenario may help explain:
Imagine a person who has been exposed to Hepatitis A is cooking your favorite meal in the kitchen of your favorite restaurant. They may feel well and fine (the incubation period of Hepatitis A is approximately 28 days (range 15–50 days)) or they may feel a bit under the weather with symptoms including fatigue, low appetite, stomach pain, nausea, and maybe jaundice-ey. Maybe this person had these symptoms for the past month or two and felt they just suffered through a really bad case of the flu or something like that. Hepatitis A is a self-limited disease that does not result in chronic infection. So the person in the kitchen may be on the mend but still very much contagious (back to work due to the financial necessity rather than being back in tip-top physical shape). During the cook’s shift, he may just feel the need to move his bowels. Pooping “on the clock” is perfectly A-OK. I mean, when you gotta go…you gotta go…especially when you feel ill. Here’s where the problem may start: Most folks do not see themselves as “dirty.” And, as you have witnessed a thousand times, either hand washing occurs, folks just skip hand washing or the hand washing was only performed for 2.3 seconds and utterly ineffective in cleaning the hands from the “cooties that may bug you.” The cook with the fecal matter fingers returns to the kitchen and puts the finishing touches on your dish. Your favorite meal arrives from your favorite restaurant having been prepared by Mr. Poopy Hands. No, there’s no visible fecal matter on his hands. There’s no pieces of poop on your dinner plate. But, there is bacterial and viral residue that clinged to the cook’s hands and therefore now clings to your burger and fries. Where does that residue end up next? Yep…in your mouth.
You Got Some Poop in your Mouth
All grossness aside, this is the way that Hepatitis A spreads. That’s what fecal-oral contamination means. Contamination may be from a less direct source such as contaminated water or other things that someone with Hepatitis A touched before you touched it followed by you inevitably touching your face somewhere before washing your own hands. And that is how doo-doo got in your mouth. No, it may not be actual pieces of stool. However, don’t fool yourself in thinking that if you ever become ill with a virus that spreads via the fecal-oral route that the “matter” which once resided in another’s butt somehow found its way into your very own mouth.
The Upside
Here’s the upside to this: Antibodies your body produces in response to the Hepatitis A infection will last for the rest of your life and protect you against ever catching Hepatitis A again (for the most part). However, contracting Hepatitis A has no real “up side.” Let’s consider the 17 folks who have died so far in Southern California out of the 569 people who became infected with Hepatitis A. Antibodies or not, these 17 (to date) will never ever get to test their brand new antibodies out. I am sure that the other 550+ infected would have liked to find a much better way to develop antibodies to Hepatitis A instead of spending nearly 2 months suffering as the infection ran (or is running) its course.
The Secret is Out
I’ve got a secret to share. There’s a way you can develop antibodies and you don’t even have to get Hepatitis A to make these cool antibodies. There’s a 2-part vaccine that’s available. I know; I am being somewhat facetious. We all know about this vaccine; it’s been around since 1995 and the results have been amazing. Check out this graph from the CDC:
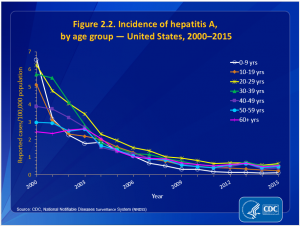
This tremendous decline in the infection rate could be attributed to good hand washing. But, let’s don’t kid ourselves. Have you ever been to a public bathroom? Do all your fellow public bathroom-users wash after handling their privates and wiping those areas that light seldom shines upon? The knowledge of the importance of handwashing has been around since the mid 19th century. We really got the message in the 80s when the CDC started a heavy hand hygiene campaign because of the increased frequency of food-borne illnesses. The message was solidified in 2009 with the swine flu scare. We know why folks should wash their hand (only many don’t “group” themselves in with “folks.” Some folks feel that their “business” is clean and everyone else’s is not-so-much).
The Decline in the Frequency of Infections
The decline in the frequency of infections is the direct response to the Hepatitis A vaccine. This 2-part “vaccination is recommended for all children age 12 months or older .” However, over the years of being a school nurse, I have had dozens and dozens of students…susceptible children… that are still not adequately immunized. Why? Do you know?
I know! I know!
There’s a bit of fear that is associated with vaccines. I hear and acknowledge these fears. Though I have my own paradigm set regarding immunizations; debating the “to immunize” or “not to immunize” is a discussion all and of its own. Let’s save that for another day. As for the proof being in the pudding, the statistics don’t fib. And, given the choice to the 569 people who became infected with Hepatitis A in Southern California in the past 11 months, what decision would they have made if they had the chance?
To Wait or Not to Wait?
This is not the best article to discuss the immunization debate. The truth is: The best way to avoid getting Hepatitis A is to become vaccinated BEFORE the outbreak. Yes, like the one is Southern California. But it’s not that simple. There are parents who truly fear vaccinating their children. If they do not vaccinate and if their children gets ill, then “nature” alone is to blame. If the parent vaccinates and the child develops an emotional disorder or some other health issue (a coincidental event), then the parent may feel responsible because it was something “they did” to their child. And, these fears are genuine. No matter what side of the fence you are on, we all can respect that kind of parent’s fear. They do not want to hurt their child.
For those who do not wish to vaccinate their children, I have this one question: If you lived in Southern California right now (Oct 2017), would you vaccinate your child? If the answer is “yes,” then consider immunizing your children now no matter where you live. Don’t wait until the cooties are attacking.
Waiting to be immunized is not necessarily the ideal plan of care for you and your children despite any possible fears you may have. To be vaccinated from the Hepatitis A virus, one will receive 2 different injection spaced out by 6 months. According to the CDC, the best time to start the Hepatitis vaccine is at one year of age. Then about 6 months later, the second vaccine is given. And, there you go.
Waiting to get vaccinated after the outbreak has begun requires that the outbreak has enough victims to be identified as an outbreak. So hundreds in a local area are already sick. Second, waiting for the outbreak to occur and then get vaccinated requires time for the vaccine to enter you body and for you body to respond to the vaccine by creating antibodies. This takes time. You have time now. Waiting…well…that just reduces your options.
The point is: If you don’t want to become sick or your children to become sick with Hepatitis A, get vaccinated.
Your information is kept private! Here’s my Privacy Statement.
References:
https://www.cdc.gov/hepatitis/statistics/2015surveillance/index.htm
https://www.cdc.gov/hepatitis/statistics/2015surveillance/pdfs/2015HepSurveillanceRpt.pdf
https://qz.com/1104305/an-unprecedented-hepatitis-a-outbreak-in-california-has-killed-17/